Group leader: Elena Tamagno
Our group is engaged in studying the cellular and molecular mechanisms related to aging that cause Alzheimer’s disease, to contribute to the development of new therapies.
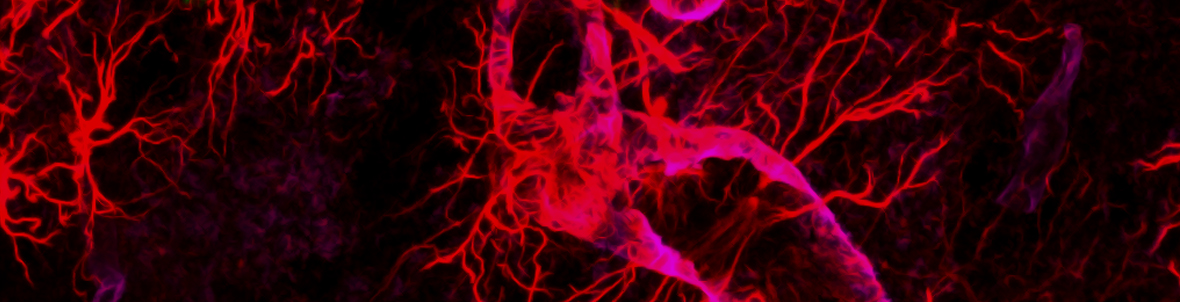
Primary neuropathological events in the pathogenesis of Alzheimer’s disease, and in all other forms of dementia, involve the aberrant formation of pathological protein species. Advances in molecular biology have provided the tools needed to unravel the mechanisms of synthesis, trafficking, and accumulation of these proteins in the brain. Research in this area has begun to produce promising clues about the role of these proteins in neural function, dysfunction and cell death and to suggest strategies to correct this molecular damage.
Our group deals with:
Study the role of oxidative stress in the hyper-regulation of β-secretase (BACE-1), enzyme involved with g-secretase in the ß-amyloid proteinproduction.
The results obtained in recent years have allowed us to relate the activity of ß-secretase to numerous risk factors such as: hypercholesterolemia, diabetes, and cerebral hypoxia; explaining the molecular mechanisms capable of determining increased amyloid beta production.
Study the relationship between sleep disorders and Alzheimer’s disease.
Numerous experimental evidence describes a bidirectional relationship between structural and qualitative sleep change and neurodegenerative disorders. Applying an experimental sleep fragmentation model to disease models and healthy models, we study brain and behavioral consequences. This study aims to clarify the role of sleep in the pathogenesis of Alzheimer’s disease and how its dysfunctions are related to a worsening of the clinical features of a dementia patient
Study the role of estrogens in the modulation of miRNA218 and the effects on conformational changes of Tau, thereforeplacing the attention on the female population that is the most accomplished by the disease.
Using animal models, we demonstrated a gender correlation between increased miRNA218 and disease progression. Currently, we have started a collaboration with the Neurology of Molinette to be able to use plasma of patients, control the levels of miRNA218 and be able to correlate them to the different stages of neurodegeneration. Finally, we are going to characterize the data obtained with the clinical pictures of patients and understand, first experimentally, whether the use of a therapy targeted to the inactivation of miRNA218 can slow the course of the disease.
Study the effect of periodic fasting in a complex laboratory model.
It is now known as calorie restriction (CR), without malnutrition, is effective in protecting the brain against aging and oxidative stress. Several studies support the theory that reducing food intake has a protectiverole against age-dependent decline in cognitive performance in Alzheimer’s disease models. We are observing the effects of periodic fasting on ß-amyloid deposition and the effect of this treatment on the Tau protein.






